Wellbeing
What Causes Low Vitamin D Levels (Even When You’re Taking Vitamin D Supplements)?
In this article, we will look at the 5 main reasons vitamin D can stay low. This is with seemingly sufficient vitamin D intake via sunshine exposure, supplementation, or diet. It’s not that vitamin D supplements don’t work; there’s something else stopping them from working. Scroll down as we uncover what causes low vitamin D and how Magnesium, Probiotics, and Glutathione supplements can help!
Table of Contents
What Happens When Your Vitamin D Is Low?
Low vitamin D levels can result in many health issues. Cancer, multiple sclerosis, rheumatoid arthritis, diabetes, cardiovascular disease, and autoimmunity are just a few examples. Vitamin D is key to healthy immune system function (1).
Vitamin D’s role in immune function involves controlling immune system inflammation and increasing the body’s ability to kill pathogens. It does this by producing the immune system signaling molecule IL-10, and the antimicrobial peptides, Defensins and Cathlicidins. Immune cells use these molecules to both find pathogens and kill them (1).
It’s no surprise that taking vitamin D supplements is a no-brainer for many people. This practice is especially common during winter when days are shorter and people spend less time outside. However, there’s a potential problem. Vitamin D levels can still stay low even when taking high-strength supplements or spending time in the sunshine.
The different forms of vitamin D
The simple flowchart below shows the different forms of vitamin D found in the body. Vitamin D precursor is turned into previtamin D3 in the skin by UVB rays from the sun. This is why sunlight is important for vitamin D production. Then, previtamin D3 is turned into cholecalciferol or vitamin D3.
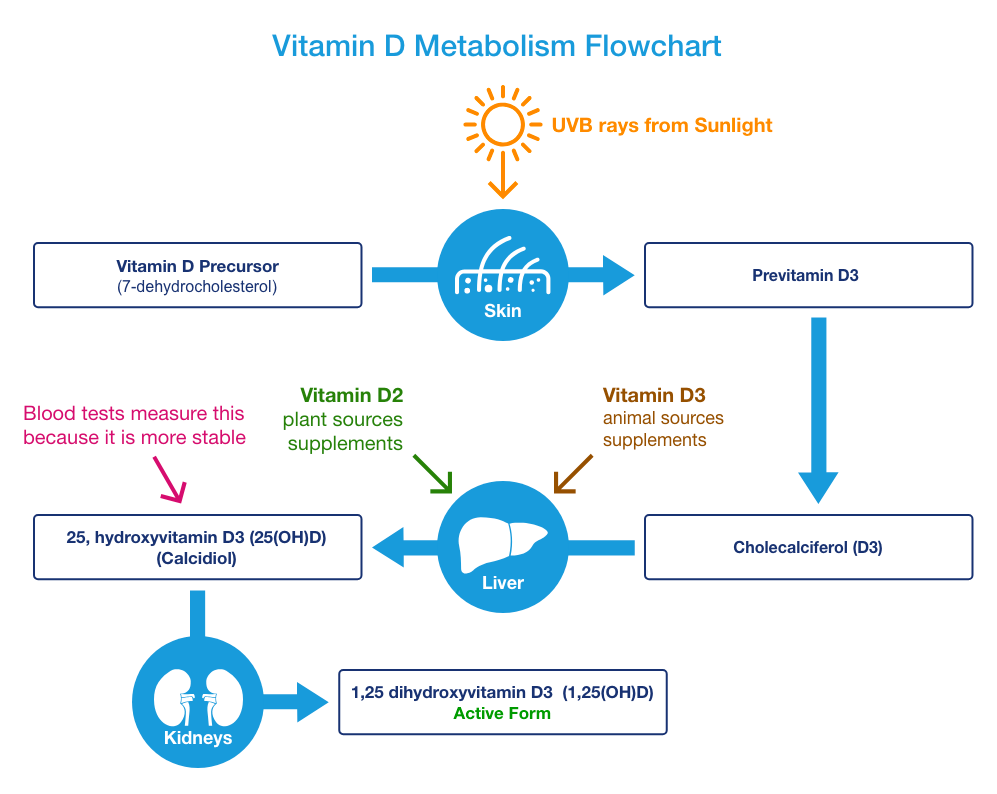
Cholecalciferol or vitamin D3 is the type we get from food or supplements (although occasionally it’s in the D2 form). By taking a supplement, we can bypass the need for sunshine to produce Vitamin D. The liver converts D3 into storage vitamin D, a.k.a. Calcidiol or 25, hydroxyvitamin D3, 25(OH)D.
The main type of vitamin D found in the blood is storage vitamin D. It’s the form commonly tested for in vitamin D tests. However, we need to turn this form into active vitamin D, a.k.a. Calcitriol or 1,25 dihydroxy vitamin D3, 1,25(OH)D.
This conversion most commonly happens in the kidneys. Active vitamin D exerts the effects we need in our tissues and, ultimately, what we need to produce.
The 5 Factors That Cause Low Vitamin D Levels
Here are the factors that cause low vitamin D in individuals:
1) Insufficient Calcium Intake
The first reason why vitamin D can stay low is insufficient calcium intake. Vitamin D is necessary to help absorb calcium in the gut.
Active vitamin D, (1,25(OH)), can do this by synthesizing the calcium-binding protein known as calbindin in the epithelial cells that line our guts.
Active vitamin D also forms the 3 types of channels through which calcium moves to be absorbed. These are known as TRPV5 and TRPV6, from the gut to the intestinal cells, and PMCA1b from the intestinal cells into the blood.
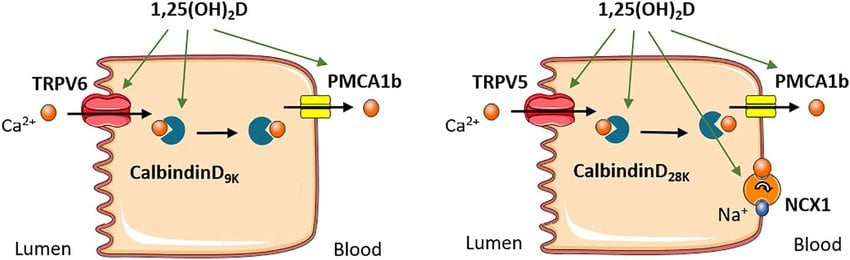
The body will use more active vitamin D to form more absorption channels if calcium levels are insufficient. This is so we get as much calcium in the gut absorbed into the body. And the outcome? Lower storage vitamin D levels in the blood.
This means less active vitamin D is available for all of its other functions in the body. By ensuring enough calcium, we can spare vitamin D for use in the immune system and for all its other functions, rather than just for calcium absorption (2, 3, 4, 5).
Problems with too much calcium
Whilst adequate calcium consumption is important, we do not recommend taking more calcium than the RDA. The RDA is the amount to aim for. What we are trying to do is to avoid not getting enough calcium.
High calcium intake can have potential health problems in itself. Excess calcium can end up in soft tissues such as the arteries causing calcification, i.e. heart disease. Because of this, we recommend avoiding high-dose calcium supplements (6).
The way to ensure you are getting the right amount of calcium is to use a calculator like this. The recommended daily allowance for calcium is 1000mg per day for most adults, although that does increase to 1200mg per pay for women over 50.
2) Magnesium
So, the 25-hydroxylase enzyme converts D2 or D3 into the storage form of vitamin D in the liver. Another enzyme, the 1-α hydroxylase enzyme, converts storage vitamin D into its active form in the kidney.
Both of these enzymes need magnesium to work. The problem is that most people, especially in the USA, don’t get enough magnesium (7).
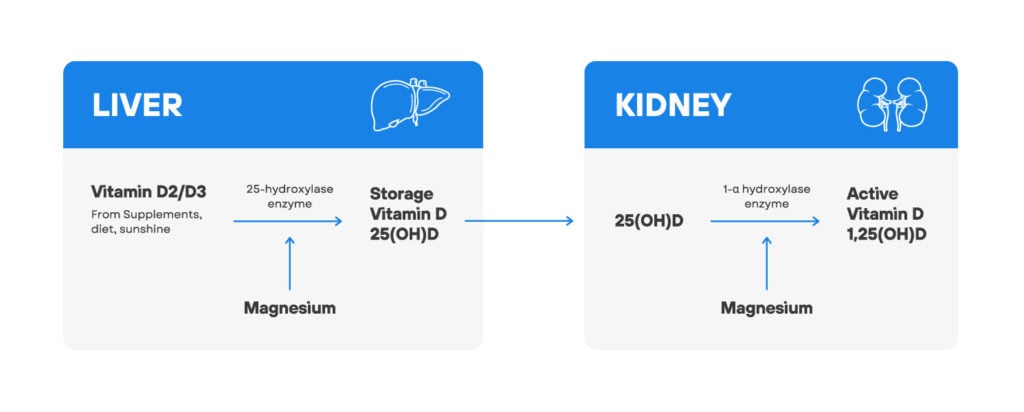
Low storage and active vitamin D levels is common in subjects with low magnesium levels. But fortunately, magnesium supplementation can reverse low vitamin D levels (8, 9).

Also, some kids suffering from rickets (a disease caused by vit. D deficiency) and low magnesium levels, will not respond to huge vitamin D doses (up to 600,000 IU daily). They only responded when supplemented with a combo of vitamin D and magnesium (10).
Further studies also show that higher magnesium intake correlates with higher storage vitamin D levels. Higher magnesium intake also lowers the risk of death from heart disease and colorectal cancer (11).
You can get extra magnesium either through the diet or relatively cheaply through magnesium supplements, such as our MagEnhance Triple Magnesium Complex.
3) Glutathione
Glutathione is the main antioxidant in the human body. Low glutathione increases oxidative stress and damage to proteins and fatty acids (12, 13).
A 2018 study showed that in both mice and humans, low vitamin D levels also correlated with low glutathione levels. Interestingly, subjects treated with glutathione or L-cysteine supplements showed increased glutathione and vitamin D levels (14).
Cysteine is used because glutathione is made of 3 amino acids, cysteine, glycine, and glutamate. Cysteine is considered the rate-limiting amino acid needed for glutathione production because there is much less available in the body than the other 2 amino acids.
The study’s authors concluded that low glutathione levels led to low vitamin D because low glutathione increased inflammation. This, in turn, leads to the downregulation of the genes responsible for producing vitamin D. Vitamin D can increase the strength of the immune response when we produce lots of it. But it can also increase the collateral damage caused by the immune system.
The body, therefore, purposely downregulates Vitamin D production during chronic inflammation. This response may occur in obese or diabetic individuals, to protect the body from further damage.
Increasing glutathione levels

You can find out your glutathione levels with a simple blood test. Anyone who wants to increase their glutathione levels, or reduce inflammation, can supplement with the glutathione precursor N-acetyl cysteine (NAC) or a Liposomal Glutathione supplement.
NAC is cheaper than Liposomal Glutathione. But as glutathione is the active form, the body doesn’t have to make any conversions. So, normally, the Liposomal Glutathione will produce better results.
If you want to supplement with glutathione, it’s important to choose the liposomal form and not the ordinary form. Liposomal forms allow glutathione to be absorbed whole. The non-liposomal form will be mostly broken down into its individual amino acids before absorption, making it much less bioavailable.
4) Fat Mass and Exercise
Increased body fat is associated with lower levels of vitamin D (15). The exact reason for this is not fully known. However, because vitamin D is a fat-soluble vitamin, it’s thought that increased body fat can cause vitamin D to be trapped in fat tissue. Excess fat in the cells leads to them becoming dysfunctional, which means they can’t efficiently release vitamin D. This means that less vitamin D is available for use in the body.
The excess fat mass may also increase levels of the enzyme 24-hydroxylase. This enzyme deactivates vitamin D and is found in high concentrations in fat tissue (16). In addition to this, because obesity creates chronic low-grade inflammation, the inflammation itself may inhibit the production of vitamin D.
People suffering from obesity can increase their vitamin D levels with supplements. But it’s been suggested they may need 2-3 times the dose as the non-obese (17).
Fortunately, lifestyle interventions that reduce body fat, such as diet changes and exercise, can increase vitamin D levels (18). Exercise breaks down fat tissues and frees up the trapped vitamin D, allowing it to enter circulation again (19).
5) Gut Microbiome/Bacteria
Vitamin D is very active in the gut cells in both calcium absorption and immune function. It’s been shown that impaired vitamin D functioning can lead to an imbalance in the gut microbiome. It can then lead to the formation of excess ‘bad bacteria’. Bacterial imbalance can lead to less vitamin D activity, creating a vicious circle (20).
Those with higher levels of active vitamin D were more likely to have ‘good bacteria’ that produce butyrate. Butyrate is a short-chain fatty acid that is used by gut cells for energy. It’s also used to reduce inflammation and to tighten the junctions between intestinal cells to prevent a ‘leaky gut’ (21, 22).

Also, it seems a lack of good bacteria only reduces active vitamin D, but storage vitamin D can remain normal. So even though the usual vitamin D tests will appear normal, there is actually a low-level vitamin D activity going on.
This means that the good bacteria are involved in turning storage vitamin D into active vitamin D. So, when testing for vitamin D levels, ask to get tested for both active and storage vitamin D (20).
Studies have shown that supplementation with probiotics can restore vitamin D activity and reduce inflammation in both mice (23) and humans (24). Probiotic supplementation with Lactobacillus rhamnosus will directly increase butyrate-producing bacteria (25).
Conclusion
So, now you know what causes low vitamin D in people. To get a full picture of your vitamin D status, we recommend testing both your storage and active vitamin D levels. If either is low, and you’re already taking supplements or spending plenty of time outside, then you can look at any of these 5 factors and see if working on them can help improve your vitamin D levels.
💬 Something on your mind? Share your thoughts in the comments. We love hearing from curious minds.
📩 And while you’re here, join our newsletter for more smart stuff (and secret perks)!
References
(1) The vitamin D-antimicrobial peptide pathway and its role in protection against infection. Gombart AF. Future Microbiol. 2009;4(9):1151-1165.
(2) A new mechanism for induced vitamin D deficiency in calcium deprivation. Clements MR, Johnson L, Fraser DR. Nature. 1987;325(6099):62-65. doi:10.1038/325062a0
(3) Increased catabolism of 25-hydroxyvitamin D in patients with partial gastrectomy and elevated 1,25-dihydroxyvitamin D levels. Implications for metabolic bone disease. Davies M, Heys SE, Selby PL, Berry JL, Mawer EB. J Clin Endocrinol Metab. 1997;82(1):209-212.
(4) The effect of dietary calcium on 1,25(OH)2D3 synthesis and sparing of serum 25(OH)D3 levels. Anderson PH, Lee AM , Anderson SM , Sawyer RK , O’Loughlin PD , Morris HA, The Journal of Steroid Biochemistry and Molecular Biology, 15 Mar 2010, 121(1-2):288-292
(5) Interaction between Vitamin D and calcium, Scandinavian Journal of Clinical and Laboratory Investigation, Paul Lips (2012) 72:sup243, 60-64
(6)The plasma membrane Ca²+ ATPase and the plasma membrane sodium calcium exchanger cooperate in the regulation of cell calcium. Brini M, Carafoli E. Cold Spring Harb Perspect Biol. 2011;3(2):a004168. Published 2011 Feb 1.
(7)Dietary intake of selected minerals for the United States population: 1999-2000. Ervin RB, Wang CY, Wright JD, Kennedy-Stephenson J. Adv Data. 2004;(341):1-5.
(8) CORRECTION OF LOW CIRCULATING LEVELS OF 1,25-DIHYDROXYVITAMIN D BY 25-HYDROXYVITAMIN D DURING REVERSAL OF HYPOMAGNESAEMIA, M. FUSS, P. BERGMANN, A. BERGANS, J. BAGON, E. COGAN, T. PEPERSACK, M. VAN GOSSUM, J. CORVILAIN, First published: July 1989
(9) Magnesium administration reverses the hypocalcaemia secondary to hypomagnesaemia despite low circulating levels of 25-hydroxyvitamin D and 1,25-dihydroxy vitamin D.Fuss M, Cogan E, Gillet C, et al. Clin Endocrinol (Oxf). 1985;22(6):807-815.
(10)Magnesium-dependent vitamin-D-resistant rickets. Reddy V, Sivakumar B. Lancet. 1974;1(7864):963-965.
(11)Magnesium, vitamin D status and mortality: results from US National Health and Nutrition Examination Survey (NHANES) 2001 to 2006 and NHANES III.Deng X, Song Y, Manson JE, et al. BMC Med. 2013;11:187. Published 2013 Aug 27.
(12)Protein carbonylation and metabolic control systems. Curtis JM, Hahn WS, Long EK, Burrill JS, Arriaga EA, Bernlohr DA.Trends Endocrinol Metab. 2012;23(8):399-406.
(13)Protein carbonyl groups as biomarkers of oxidative stress. Dalle-Donne I, Rossi R, Giustarini D, Milzani A, Colombo R.Clin Chim Acta. 2003;329(1-2):23-38.
(14) Glutathione Stimulates Vitamin D Regulatory and Glucose-Metabolism Genes, Lowers Oxidative Stress and Inflammation, and Increases 25-Hydroxy-Vitamin D Levels in Blood: A Novel Approach to Treat 25-Hydroxyvitamin D Deficiency. Jain SK, Parsanathan R, Achari AE, Kanikarla-Marie P, Bocchini JA Jr. Antioxid Redox Signal. 2018;29(17):1792-1807.
(15) Fat Mass Is Associated with Serum 25-Hydroxyvitamin D Concentration Regardless of Body Size in Men, Kyung-Jin Yeum, Bess Dawson-Hughes, and Nam-Seok Joo, Nutrients. 2018 Jul; 10(7): 850.
(16) 1alpha,25-Dihydroxyvitamin D hydroxylase in adipocytes.Li J, Byrne ME, Chang E, et al. J Steroid Biochem Mol Biol. 2008;112(1-3):122-126.
(17) Impaired Release of Vitamin D in Dysfunctional Adipose Tissue: New Cues on Vitamin D Supplementation in Obesity.Di Nisio A, De Toni L, Sabovic I, et al. J Clin Endocrinol Metab. 2017;102(7):2564-2574.
(18) Relationships between circulating 25(OH) vitamin D, leptin levels and visceral adipose tissue volume: results from a 1-year lifestyle intervention program in men with visceral obesity. Gangloff A, Bergeron J, Lemieux I, et al. Int J Obes (Lond). 2020;44(2):280-288.
(19) Mobilising vitamin D from adipose tissue: The potential impact of exercise. Hengist A, Perkin O, Gonzalez JT, et al. Nutr Bull. 2019;44(1):25-35.
(20) Vitamin D metabolites and the gut microbiome in older men. Thomas RL, Jiang L, Adams JS, et al. Nat Commun. 2020;11(1):5997. Published 2020 Nov 26.
(21) Butyrate Enhances the Intestinal Barrier by Facilitating Tight Junction Assembly via Activation of AMP-Activated Protein Kinase in Caco-2 Cell Monolayers, Luying Peng, Zhong-Rong Li… J Nutr. 2009 Sep; 139(9): 1619–1625.
(22) Effects of oral butyrate supplementation on inflammatory potential of circulating peripheral blood mononuclear cells in healthy and obese males. Cleophas MCP, Ratter JM, Bekkering S, et al. Sci Rep. 2019;9(1):775. Published 2019 Jan 28.
(23) Vitamin D receptor pathway is required for probiotic protection in colitis. Wu S, Yoon S, Zhang YG, et al. Am J Physiol Gastrointest Liver Physiol. 2015;309(5):G341-G349.
(24) Bolus Weekly Vitamin D3 Supplementation Impacts Gut and Airway Microbiota in Adults With Cystic Fibrosis: A Double-Blind, Randomized, Placebo-Controlled Clinical Trial. Kanhere M, He J, Chassaing B, et al. J Clin Endocrinol Metab. 2018;103(2):564-574.
(25) Lactobacillus rhamnosus GG-supplemented formula expands butyrate-producing bacterial strains in food allergic infants. Berni Canani R, Sangwan N, Stefka AT, et al. ISME J. 2016;10(3):742-750.




