Nootropics
Thiamine (Vitamin B1): A Potent Energy Booster and Anti-Beriberi!
Today, you’ll learn why we added Thiamine, an energy booster and anti-beriberi vitamin, to our Seneca Nootropic Complex. We’ll also give you an overview of the circumstances surrounding its discovery.
Table of Contents
What is Thiamine?
Thiamine (or vitamin B1) helps with energy and cellular metabolism as well as many other important functions in the body. It’s an essential vitamin, so the body cannot make it on its own. We can get B1 from food or supplements (scroll down to see our infographic on the best thiamine food sources).
The body only stores a small amount of B1 (around 30mg), particularly in tissues like the heart, liver, brain, kidney, and skeletal muscles. Its half-life is between 9-18 days, so it’s important to get this vitamin regularly, preferably daily (1).
Vitamin B1 is on the World Health Organization’s List of Essential Medicines (2). This list contains the medications and nutrients that are safe, effective, and essential for a health system.
How was Vitamin B1 discovered?
Vitamin B1 is found in a staple food that’s found in many countries – RICE. In the 19th century, rice milling became widespread. Eating “white” rice – with its husk, bran, and germ removed – became a popular diet trend in Japan (3).
Unfortunately, this switch from healthier brown rice to polished white rice also caused a rapid acceleration in the number of beriberi cases. Beriberi makes walking difficult and causes a loss of feeling and muscle function, mental confusion, strange eye movements, nerve damage, and heart failure. The disease was so widespread it was considered endemic to Japan.
Beriberi and the Japanese navy
Beriberi was such a huge problem for Japanese sailors, they were dying of it in record numbers. It was first thought to be infectious. But the naval physician Kanehiro Takaki thought it had something to do with the sailors’ diet of plain white rice. So, he conducted a diet experiment to find out once and for all. He fed one group of sailors only white rice. A second group had a more nutritionally complete diet of white rice, barley, beans, meat, and fish.
Guess which group had zero cases of beriberi?
The second group, of course. Well, technically, 14 crew members from the second group developed the disease. But that was because they didn’t follow their prescribed meal plan. Instead, they secretly continued eating white rice only…
That said, the most significant finding of Takaki’s experiment was in the white rice group. More than half of them suffered from beriberi! This was a significant discovery because it was the first step toward eradicating beriberi in the navy, and the whole of Japan. Because of his discovery, Takaki was made a baron by the Japanese empire (4).
But it wasn’t until 1911 when Casimir Funk finally isolated thiamine from rice bran. He described it as the X-factor in preventing and treating beriberi (5). A few more decades went by before Robert Williams finally synthesized thiamine, which made it possible to fortify foods with thiamin around the world (6).

What Does Thiamine Actually Do in the Body?
In addition to its proven anti-beriberi benefits, here are some other benefits of adding more Vitamin B1 thiamine to your diet:
1) Thiamine contributes to energy production
Thiamine helps convert carbohydrates into glucose. Thiamine is one of the 5 cofactors needed for the enzymes Pyruvate Dehydrogenase Complex (PDC) and α-Keto Glutarate Dehydrogenase Complex (α-KGDC) (1).
Firstly, the PDC enzyme is needed to turn sugar into energy. Glucose and fructose (both sugars) can enter a process called glycolysis which occurs in the cytosol of the cell. As shown in the image below, glycolysis is the process that converts sugar (glucose) into Acetyl-CoA.
Next, the Acetyl-COA goes through the ‘Krebs cycle’ which leads to energy production. The α-KGDC enzyme is instrumental here in that it helps produce Succinyl-COA.
2) It helps with Myelin Sheath formation
As we can see from the above diagram, Acetyl CoA is also necessary for the formation of myelin. Myelin is a fat-based molecule that surrounds the axons of nerve cells. These are the long thin parts of nerve cells that connect the two ends and transmit electrical signals.
The myelin provides insulation to the axons, and there are gaps between sections of the myelin. These gaps allow electrical impulses to jump down the axons between the gaps. This means signals can move along neurons, much more quickly than if there was no myelin sheath.
Diseases such as Multiple Sclerosis involve a reduced ability to produce myelin. And subsequently, the symptoms involve movement issues related to an inability to send nerve impulses to the muscles efficiently.
3) It is a cofactor in the Pentose Phosphate Pathway (PPP)
The PPP is a metabolic pathway that helps produce DNA, RNA as well as NADPH, which help make the body’s main antioxidant, Glutathione. It also helps with fatty acids, steroid hormones, neurotransmitters, and amino acids. The PPP uses about 5-10% of the body’s glucose.
Benfotiamine, a fat-soluble version of thiamine, may help diabetics support the disposal of sugar down the PPP pathway. It offers better absorption by the brain and central nervous system, and can increase body stores of B1. This potentially means that diabetics can efficiently use excess glucose and reduce blood sugar levels (7).
4) Vitamin B1 promotes insulin sensitivity
Research studies have shown a relationship between diabetes and thiamine levels. Compared to healthy individuals, diabetics have lower thiamine levels (8):
- Type 1 diabetics – 76% lower thiamine levels
- Type 2 diabetes – 50-75% lower thiamine levels
Fortunately, increasing thiamine dosage may help manage diabetic symptoms. One study reported that 100mg of thiamine given 3x a day for 90 days yielded promising results. This dosage was enough to reduce the severity of symptoms in type 2 diabetics who also had microalbuminuria (9).
5) Thiamine supports optimal heart health
Thiamine also contributes to the normal function of the heart. A deficiency of this essential nutrient can lead to congestive heart failure (10).
One study reported that thiamine supplementation helped improve the left ventricular ejection fraction (LVEF) in patients with congestive heart failure (11).
LVEF measures the blood pumped out of the heart’s left ventricle with each contraction. Simply put, patients with congestive heart failure have less than normal ejection fraction rates. Normal LVEF rates range from 55 to 70% (12).
6) Vitamin B1 supports brain health
The brain is highly vulnerable to vitamin B1 deficiency. After all, B1 contributes to energy, glutathione, fatty acids, neurotransmitters, and amino acid production.
Also, thiamine supplementation may help with the following conditions:
Wernicke-Korsakoff Syndrome (WKS)

Excessive alcoholism can prevent B1 absorption, thus leading to severe thiamin deficiency. Alcoholism is the main risk factor for WKS, a rare brain disorder. WKS signs and symptoms include (13):
- Double vision
- Loss of muscle coordination
- Confusion
- Memory loss
- Difficulties in communicating
- Hallucinations
So, can thiamine supplementation help with WKS?
According to a 2017 study, high-dose thiamine is a safe and effective treatment option. Researchers administered at least 500mg of intravenous thiamine to a small group of patients (n=11) with suspected Wernicke encephalopathy. After a few days (median is 3 days), 8 out of 11 patients showed significant improvements in their WE symptoms (14).
Stroke patients
A stroke occurs when the blood supply to the brain is cut off. It affects vision, speech, and movement. Another poststroke effect is fatigue, which isn’t always improved with rest (15). But thiamine supplementation might help!
In one case study, 3 stroke patients suffering from poststroke fatigue were given a high dose of thiamine. Two patients were given 600mg/day orally. The third patient was given 100mg/week parenterally. The researchers observed a significant reduction in all 3 patients’ fatigue levels after supplementing with thiamin for several months (16).
Neurodegenerative conditions
Vitamin B1 therapy offers neuroprotection and helps slow down the advance of neurodegenerative diseases like Alzheimer’s, Parkinson’s, and Huntington’s (17).
Patients suffering from Alzheimer’s have reduced levels of thiamine in the brain. The activity of thiamin-dependent enzymes also slows down. However, the good news is that thiamin supplements may help improve cognitive function, especially in younger patients. Unfortunately, elderly patients have naturally lower vitamin B1 absorption rates because of their age, so higher doses are recommended. Studies suggest an initial dosage of 100mg 2-3 times a day for at least 1-2 weeks (18).
Parkinson’s is another common neurodegenerative condition among older individuals. According to Luong and Nguyen, thiamine induces the release of dopamine and may help improve Parkinson’s symptoms as well (19).
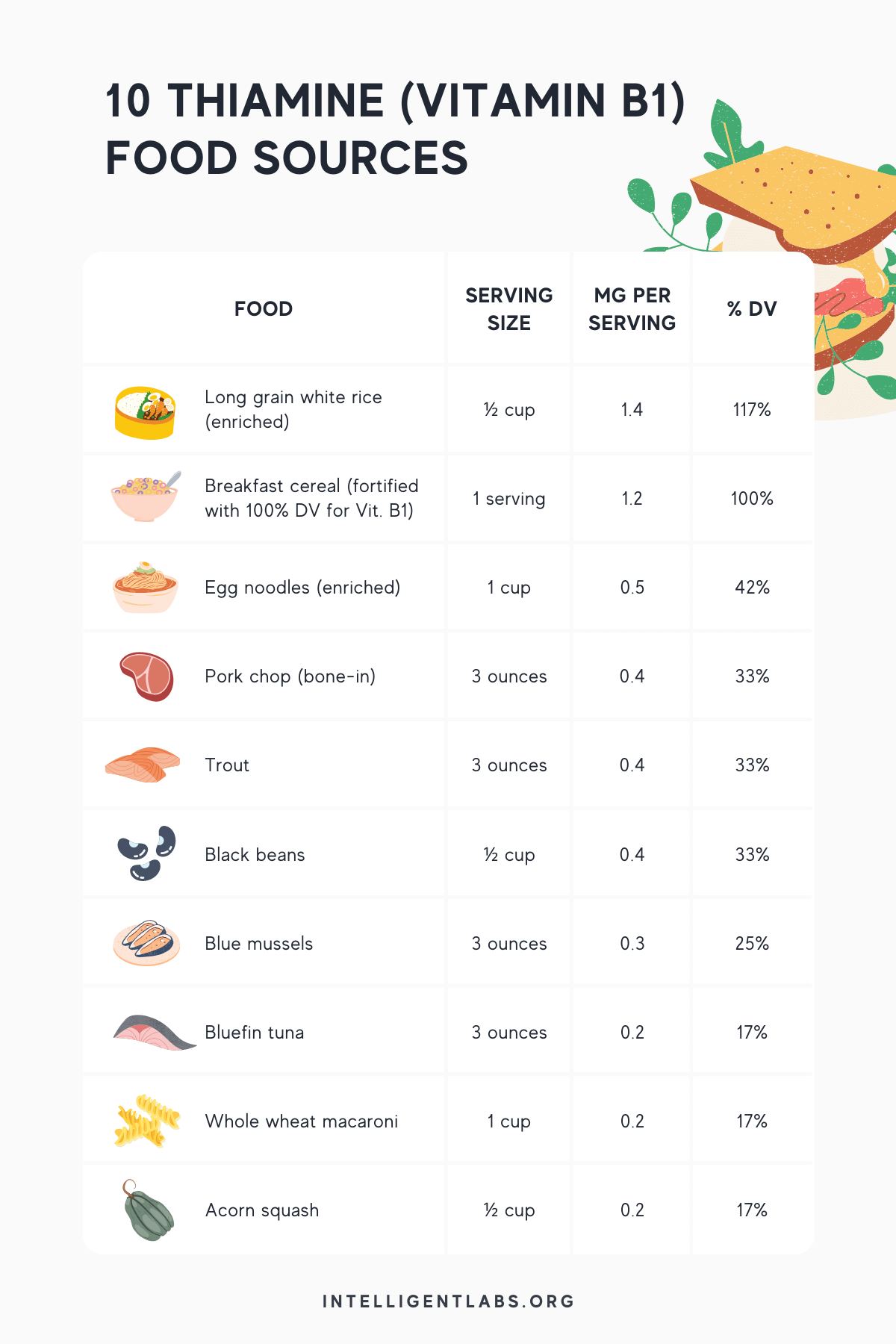
What are the best food sources of Thiamine?
To ensure you meet the required daily allowance for Vitamin B1 (please refer to the next section), consider eating more of these thiamin-rich foods (20):
What’s the best Vitamin B1 Thiamine dosage?
Here’s the recommended daily allowance (RDA) for adults:
- Men 19 years old and above: 1.2mg
- Women 19 years old and above: 1.1mg
- Pregnant and lactating women: 1.4mg
Is there an upper limit?
To date, no upper limit for thiamine has been set. B1 is considered safe and non-toxic. No reports of bad effects from high doses have been noted so far.
Final words
Thiamine is one of the ingredients in our Seneca Nootropic complex. Each serving of Seneca contains 1.1mg of Thiamine. This dose is sufficient to complement the health benefits of the other B vitamins (B2, B3, B6, B9, and B12) as well as the remaining compounds present in Seneca.
To know more about nootropics, click here to read our article on “What are nootropics and cognitive enhancing supplements?”
References
(1) Vitamin B1 (Thiamine), Julianna L. Martel; Connor C. Kerndt; Harshit Doshi; David S. Franklin, StatPearls [Internet].
(2) WHO Model Lists of Essential Medicines; https://www.who.int/groups/expert-committee-on-selection-and-use-of-essential-medicines/essential-medicines-lists
(3) DEADLY WHITE RICE IN JAPAN’S HISTORY, Yasuka, March 8, 2018.
(4) Kanehiro Takaki and the control of beriberi in the Japanese Navy, Yoshifumi Sugiyama and Akihiro Seita Volume 106, Issue 8.
(5) Casimir Funk, Anna Piro, Giuseppe Tagarelli, Paolo Lagonia, Antonio Tagarelli and Aldo Quattrone, Annals of Nutrition & Metabolism Vol. 57, No. 2 (2010), pp. 85-88 (4 pages)
(6) How Sick Chickens and Rice Led Scientists to Vitamin B1, Sarah Laskow, OCTOBER 30, 2014
(7) The multifaceted therapeutic potential of benfotiamine, Pitchai Balakumar, Ankur Rohilla, Pawan Krishan, Ponnu Solairaj, Arunachalam Thangathirupathi, Pharmacol Res. 2010 Jun;61(6):482-8.
(8) Blood thiamine and its phosphate esters as measured by high-performance liquid chromatography: levels and associations in diabetes mellitus patients with varying degrees of microalbuminuria, O S Al-Attas, N M Al-Daghri, A A Alfadda, S H Abd-Alrahman, S Sabico, J Endocrinol Invest . 2012 Dec;35(11):951-6.
(9) High-dose thiamine therapy for patients with type 2 diabetes and microalbuminuria: a randomised, double-blind placebo-controlled pilot study, N Rabbani, S S Alam, S Riaz, J R Larkin, M W Akhtar, T Shafi, P J Thornalley, Diabetologia . 2009 Feb;52(2):208-12.
(10) Effects of thiamine on cardiac function in patients with systolic heart failure: systematic review and metaanalysis of randomized, double-blind, placebo-controlled trials, James J Dinicolantonio, Carl J Lavie, Asfandyar K Niazi, James H O’Keefe, Tian Hu, Ochsner J . 2013 Winter;13(4):495-9.
(11) Ejection Fraction, reviewed by a Cleveland Clinic medical professional, https://my.clevelandclinic.org/health/articles/16950-ejection-fraction
(12) Thiamine Supplementation for the Treatment of Heart Failure: A Review of the Literature, James J. DiNicolantonio PharmD, Asfandyar K. Niazi, Carl J. Lavie MD, James H. O’Keefe MD, Hector O. Ventura MD, Congestive Heart Failure Volume 19, Issue 4 p. 214-222
(13) Alcohol-Related Neurologic Disease, Medically reviewed by Seunggu Han, M.D. — By Jacquelyn Cafasso.
(14) High-dose Parenteral Thiamine in Treatment of Wernicke’s Encephalopathy: Case Series and Review of the Literature, Andrew Nishimoto, Justin Usery, John C Winton, Jennifer Twilla, In Vivo . 2017 Jan 2;31(1):121-124.
(15) Fatigue and tiredness, from: https://www.stroke.org.uk/effects-of-stroke/tiredness-and-fatigue
(16) High-Dose Thiamine Improves Fatigue After Stroke: A Report of Three Cases, Antonio Costantini, Maria Immacolata Pala, Maria Lucia Catalano, Cristiano Notarangelo, and Pamela Careddu, The Journal of Alternative and Complementary Medicine, Vol. 20 No. 9
(17) [The role of thiamine in neurodegenerative diseases] Irena Bubko, Beata M Gruber, Elżbieta L Anuszewska, Postepy Hig Med Dosw (Online) . 2015 Sep 21;69:1096-106.
(18) Role of Thiamine in Alzheimer’s Disease Khanh vinh quốc Lu’o’ng, Lan Thi Hoàng Nguyễn, American Journal of Alzheimer’s Disease & Other Dementias®
(19) The Beneficial Role of Thiamine in Parkinson Disease, Khanh v. q. Lương, Lan T. H. Nguyễn, CNS Neuroscience & Therapeutics, Volume 19, Issue 7 p. 461-468
(20) Thiamin Fact Sheet for Health Professionals, from: https://ods.od.nih.gov/factsheets/Thiamin-HealthProfessional/#en52