Probiotics
Probiotics for UTI – Can Probiotics Help Prevent Urinary Tract Infections?
Count yourself lucky if you’ve never had urinary tract infection or UTI in your life. On the pain scale, I’d personally give it a 6 or 7, but on the annoyance scale, I’d definitely give it a 10! Going to the bathroom every 10 minutes to pee only a few drops each time is the most annoying thing ever. Now, antibiotics can get rid of a UTI fairly quickly, but it’s got a number of downsides, too. Today, you’ll learn why probiotics for UTI is a much better, more natural treatment option.
Table of Contents
What’s a UTI anyway?
For those that haven’t had UTI before (or weren’t aware you had it), here’s a primer to get you up to speed. Basically, UTI’s are bacterial infections that can occur at any point of the urinary tract – from the urethra, bladder, ureter, and all the way up to the kidneys.
Infections at any of these urinary system components go by different names:
- Urethritis – infection in the urethra
- Cystitis – infection in the bladder
- Pyelonephritis – infection in the kidney, or very rarely, the ureter (the tube which carries urine from the kidney to the bladder)
These different infections become more serious as bacteria goes from the urethra to the kidney. It’s very important to treat it right away to prevent it from progressing. Currently, antibiotics are commonly used to treat these infections. But later on, you’ll learn why probiotics for UTI are a much better alternative.
Now that you know what UTI’s are, here’s a not-so-fun fact (especially if you’re a woman):
With the way the female anatomy is designed, women literally get the short end of the stick. What I mean by that is, the female urethra is shorter than male ones, so women are naturally more prone to UTI’s than guys.
That being said, over 50% of women get a UTI in their lifetime, and for 25% of them, the infection reoccurs and significantly impacts their quality of life (1, 2). Of course, UTI’s can also affect men (even with their longer urethras), but the infection rate is 50 times less common than in women.
Common UTI symptoms
Whether or not you belong to the fairer sex, it’s important to know what to look for to find out if you have an infection. The last thing you want is for a relatively mild urethritis or cystitis to escalate to a potentially life-threatening infection – all because you ignored these common UTI symptoms below!
- Dysuria – pain when urinating
- Frequent or urgent need to urinate (of often tiny amounts)
- Nocturia – frequently needing to go at night
- Abnormal urine color usually with a strong smell
- Hematuria or pyuria– blood or pus in the urine
- Lower back or abdominal pain
These symptoms are unpleasant, but they are not considered serious. However, if the infection does spread to the kidneys (pyelonephritis), it can potentially cause kidney damage or even death. So, get yourself checked out if you do experience these symptoms.
What causes UTI’s?
Have you heard of the phenomenon known as ‘honeymoon cystitis’? This frequently occurs amongst new brides right after they come back from their honeymoons. And you know what’s the most common culprit?
No, it’s not their grooms (not technically anyways) … but the bacteria called Escherichia coli (or E. coli for short). Yes, it’s that bacteria that infamously lives in our colon (that’s our backsides).
Most cases of UTI’s (around 80%) are caused by E. coli (5-7). But sometimes in women, the bacteria can also be transferred from the vagina (1-4).
E. coli lives naturally in our gastrointestinal (GI) tract, a.k.a. the gut, although only in small numbers (2). However, when the growth levels of E. coli increase beyond what’s normal, and they get off balance with the good bacteria, it can start to cause problems for us (8).
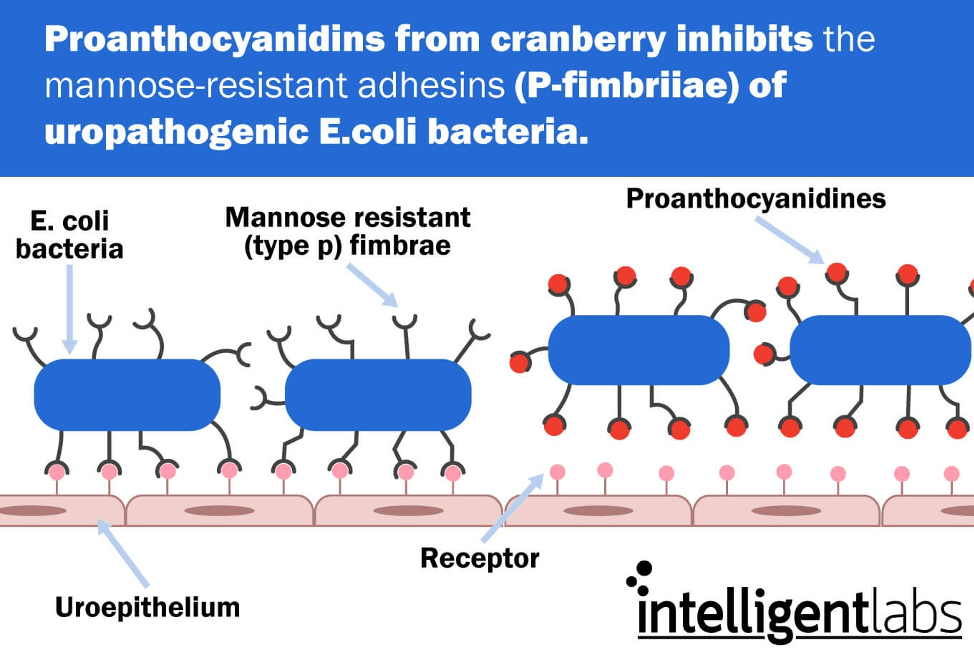
Here’s a graphic illustrating how E. coli can cause UTI’s:
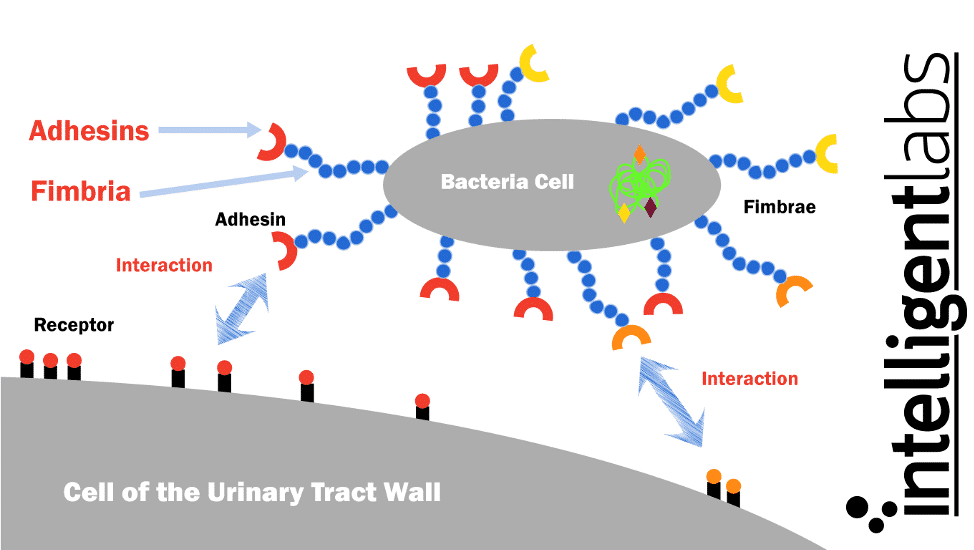
E. coli have special finger-like projections called fimbriae, which are sticky and made of a glycoprotein called lectin. Lectin allows the fimbriae to stick to the cell walls of our urinary tract (9). The ends of the fimbriae have sticky proteins called adhesins that stick to receptors on the cells lining the urinary tract.
Although the urinary system is designed to keep out such microscopic invaders, these defenses sometimes fail. If enough E. coli gets into the urinary tracts and stick to the cells, they can multiply and colonize there, which causes an infection.
The problem with current UTI treatment options
The standard treatment for a UTI is a course of antibiotics, and it’s been this way for many years. Antibiotics can still effectively treat uncomplicated UTI’s, but here’s the alarming truth:
- The occurrence of bacteria that are causing UTI infection and are also resistant to antibiotics are growing (10).
- And perhaps more worryingly, even when antibiotics do cure the infection, it can negatively impact other aspects of our health.
The main issue here is that antibiotics don’t just kill UTI-causing bacteria like E. coli, it also kills off beneficial bacteria in our gut. Then, as the bacterial populations regrow after a course of antibiotics is over, it can cause ‘dysbiosis’.
Dysbiosis is an overgrowth of potentially pathogenic bacteria, fungi, and other microbes. This can directly lead to fungal infections like thrush (both oral and vaginal), candida overgrowth, and other GI infections, most notably Clostridium difficile (11).
However, dysbiosis has also been linked with many other health conditions. These include skin problems, mental health issues like anxiety and depression, immune conditions, and obesity (12).
With such a long list of possible side effects, would you still be willing to use antibiotics to treat a urinary infection? I wouldn’t blame you if say no. So, let’s find out in the next section if probiotics for UTI is indeed the best natural alternative to antibiotics!

How to treat UTI’s without antibiotics?
So, because of the problems with antibiotic treatment and the increase of antibiotic-resistant strains of bacteria, this form of treatment is becoming less and less effective. Going forward, UTI prevention is a significant treatment goal, especially for people who suffer from recurrent infections (13).
Now, there are 3 major areas we can focus on to help prevent – and treat – UTI’s.
1st Step: Take care of your hygiene to prevent UTI’s
As the saying goes, prevention is better than cure. Follow these basic hygiene rules to stop bacteria from the colon or vagina from reaching the urethra.
- Urinate when you feel the need to go, and don’t resist the urge.
- Wipe from front to back in the bathroom, so you are preventing bacteria from entering your urethra.
- Take showers instead of tub baths, and avoid hot tubs/Jacuzzis.
- If you can, cleanse your genital area before and after having sexual intercourse, and try to urinate as well.
- Avoid using feminine hygiene sprays, which may irritate your urethra.
- Also avoid vaginal douching as this can damage the microbial balance in the vagina. Doing so can lead to an increase in pathogenic bacteria that could be transferred to the urethra. Moreover, it can also increase the chance of vaginal yeast and bacterial infections.
2nd Step: Take probiotics for UTI prevention
Probiotics (a.k.a. good bacteria) help keep the gut healthy. It restores normal gut bacterial balance, and ensures E. coli and other pathogenic bacteria are under control. But where exactly can you find probiotics?
Well, fermented foods naturally contain probiotics. A few examples are yogurt, pickles, miso, sauerkraut, kimchi, some kinds of cheese, and sourdough bread. These are all delicious foods, but when it comes to UTI prevention, there’s a better option – probiotic capsules!
Studies show that probiotic capsules taken orally can change not just the bacterial balance in the gut, but also in the vagina. This is obviously great news for all the women out there!
Now, the thing is there is a close correlation between a change in the normal microbiota (i.e. bacterial balance) in the vagina and an increased likelihood of developing a UTI (14). And since the vagina’s microbiome is predominantly made up of Lactobacillus strains, it’s therefore not all that surprising that Lactobacillus probiotic capsules (taken orally) can replenish the vaginal microbiome (15, 16).
Here are some notable findings:
In Finland, a study showed that drinking kefir (fermented milk containing probiotics) 3 times a week reduced UTI’s (17).
Another study tested probiotic supplements against antibiotics for a year in a group of women who suffered from recurrent UTI’s. They found that in women who were given antibiotics for a year, the average number of UTIs went down from 7 to 2.9. For women given probiotics, the average number went down from 6.8 to 3.3 (18).
The difference may not look all that significant, but here’s the thing:
In women with ‘complicated UTI’s’* the probiotic group did better, experiencing only 3.4 recurrences as opposed to 4.4 in women taking antibiotics.
*Complicated UTIs were defined as UTIs in women with functional or structural abnormalities of the urinary tract, metabolic and/or hormonal abnormalities, or impaired host responses.
Also, rather disturbingly, the women taking antibiotics increased the amount of antibiotic-resistant E. coli that they carried to between 80% and 95% of the total amount. In contrast, the probiotic group experienced no increase in antibiotic-resistant bacteria.

3rd Step: Take cranberry juice and D-mannose powder
So we’ve already seen that supplementing with probiotics for UTI is virtually as effective as antibiotics for preventing infections. And probiotics can reduce them by over 50% with none of the dangerous side effects of antibiotics.
With proper hygiene practices, we can reduce this even more, but what if we took it to another level? We can do this by also supplementing with cranberry juice and D-mannose.
Cranberry juice has long been used as a home remedy to treat UTI’s. It was initially believed that cranberries somehow made the urine more acidic, which made it difficult for infectious bacteria to grow there (19).
However, we now understand that cranberry juice works because it contains 2 compounds that stop the E. coli bacteria from being able to stick to the cells lining the urinary tract (known as uroepithelial cells) (20).
These are the 2 compounds found in cranberry juice:
- D-mannose – it’s a naturally occurring sugar known as mannose sensitive
- Proanthocyanidin (or PAC for short) – a condensed tannin that is mannose resistant
Here’s an illustration on the mechanism of D-mannose against UTI-causing bacteria:
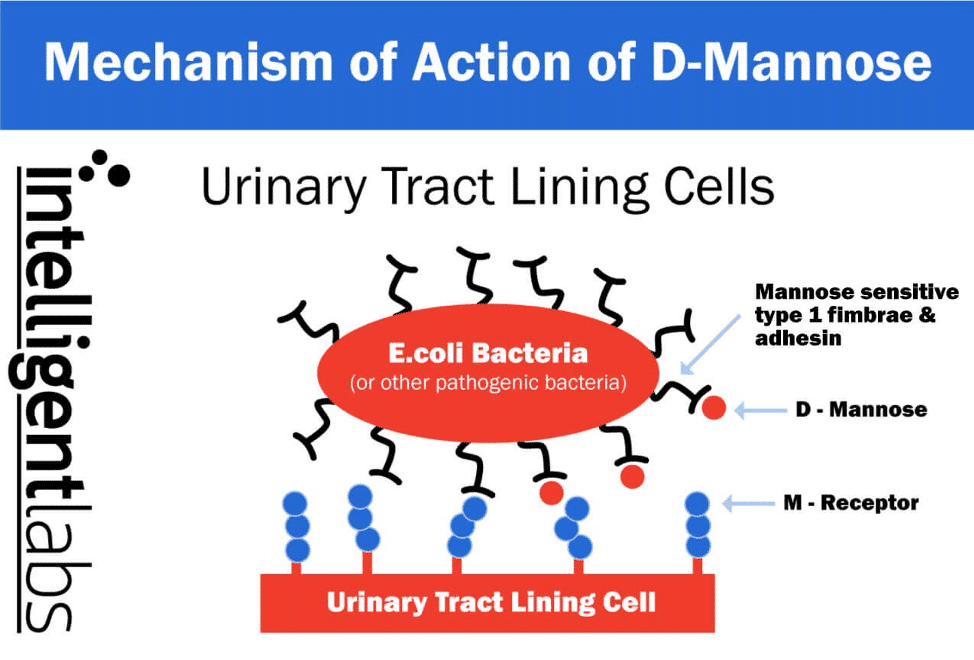
As seen in the first image above, there are finger-like projections that come from the E. coli bacteria called fimbriae that the E. coli use to stick onto the cells on the walls of the urinary tract. They use the small sticky adhesins at the end of their fingers to do the ‘sticking.’ These adhesins are either mannose sensitive (type 1) or mannose resistant (P fimbriae).
Because D-mannose is ‘mannose sensitive’, it plugs itself in the mannose sensitive (type 1) adhesins to stop them sticking to the cells of the urinary tract walls. And because the Proanthocyanidin is ‘mannose resistant’ it can plug itself into the mannose resistant (P fimbriae) adhesins.
Although D-mannose is a component of cranberry juice, it is recommended to take it as a separate pure D-mannose powder as this makes it 10-50 times stronger than the D-mannose in cranberry.
Also, although D-mannose is sugar, it is completely safe to take for long term because very little of it is metabolized. It also doesn’t interfere with blood sugar regulation, even for diabetics (21).
Studies on the effectiveness of cranberry juice and D-mannose to prevent UTI’s
There have been several studies showing the effectiveness of either cranberry juice powder or pure D-mannose powder in preventing UTI’s. Here are some of them:
Study 1:
Walker et al (22) found in their experiment that women (who were taking Cranberry Juice powder) had, on average, 2.4 UTIs per year, while those taking a placebo averaged 6 UTI’s a year.
Study 2:
A study conducted on sexually active women between 21 and 72 years of age. 150 women were put into 3 groups: one group drank cranberry juice, another took cranberry capsules, and the third group took a placebo (23). The researchers found the following:
- 32% of the placebo group suffered 1 or more UTIs in the year
- 20% of the group that drank cranberry juice suffered one or more UTI’s
- Only 18% of the group taking cranberry capsules suffered 1 or more UTI
Study 3:
Another study on pure D-mannose powder, conducted on 308 women after they had recovered from acute cystitis, gave them either D-mannose, antibiotics, or a placebo (24). They found the following:
- 61% of women in the placebo group developed a recurrent UTI
- 4% in the antibiotics group developed a recurrent UTI
- Only 14.5% of the D-mannose group developed a recurrent UTI
The winning formula: Cranberry juice + probiotics for UTIs
Probiotics, cranberry juice powder, and pure D-mannose powder have all shown their effectiveness at reducing UTI’s. Multiple studies show that cranberry juice powder and D-mannose are actually more effective at preventing UTIs than antibiotics. And probiotics have many health benefits outside of preventing UTI’s and are a vital part of any health regimen.
Now, is there such a product that combines ALL THREE UTI-fighting ingredients – probiotic, cranberry juice powder and pure D-mannose powder?
Yes, there is! Here at Intelligent Labs, we’ve created the perfect probiotic supplement for women (yes, men can take it, too). We’ve combined the highest quality probiotics (patented probiotic strains produced by Dupont), with organic cranberry juice powder and pure D-mannose powder. The supplement is formulated not only to help prevent UTI’s, but also to maximize mental and physical health!
Here’s a bottle of our Women’s Probiotics and Prebiotics Supplement with Sunfiber and FOS:
Each capsule contains the prebiotics Sunfiber® & FOS. Prebiotics are non-digestible fibers that act as food for probiotics. These fibers essentially nourish the probiotics when they are in the capsule and in your gut. This helps ensure the probiotics are still alive when you take them and successfully reproduce in the gut.
Then finally, we use an Activ-Polymer™ bottle, which features an impenetrable desiccant sleeve wrapped around the probiotic to ensure they are virtually moisture-free. The Oxyfree® desiccant absorbs any oxygen and removes any residual moisture from inside the bottle. This is because probiotics will degrade whenever they are exposed to moisture and oxygen, and we do our utmost to ensure the probiotics reach you in perfect condition.
Ready to use probiotics for UTI treatment?
Probiotics for UTI work great at treating urinary tract infections. However, it’s the 3-in-1 combo of probiotics, cranberry juice powder and D-mannose powder that offers the best results against UTI’s. Intelligent Labs’ women’s probiotics supplement contains all three ingredients – it’s specifically formulated to help prevent and treat UTI’s in women.
Have you tried our special probiotics for women? Let us know what you think in the comments below!
References
- Scholes D, Hooton TM, Roberts PL, Stapleton AE, Gupta K, Stamm WE. 2000. Risk factors for recurrent urinary tract infection in young women. J Infect Dis. 182(4):1177-82.
- Howell A, B. 2007. Bioactive compounds in cranberries and their role in prevention of urinary tract infections. Mol. Nutr. Food Res. 51. P:732-737
3.Scholes D, Hooton TM, Roberts PL, Stapleton AE, Gupta K, Stamm WE. 2000. Risk factors
for recurrent urinary tract infection in young women. J Infect Dis. 182(4):1177-82.
- Howell A, B. 2007. Bioactive compounds in cranberries and their role in prevention of urinary tract infections. Mol. Nutr. Food Res. 51. P:732-737.
- Ronald A. 2003. The etiology of urinary tract infection: traditional and emerging
pathogens. Dis Mon. 49(2):71-82. - Nicolle LE. 2008. Uncomplicated urinary tract infection in adults including uncomplicated
pyelonephritis. The Urological Clinics of North America. 35(1):1–12, v. - Gupta K, Scholes D, Stamm WE. 1999. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA (The Journal of the American Medical Association). 281(8):736-8.
- Cartwright P. 2011. Probiotic Allies. How to Maximise the Health Benefits of your
Microflora. Prentice Publishing, Ilford. pp85-87. - Ofek I, Goldhar J, Zafriri D, Lis H, Adar R, Sharon N. 1991. Anti-Escherichia coli adhesin activity of cranberry and blueberry juices. N Engl J Med. 324(22):1599.
- Gupta K, Scholes D, Stamm WE. 1999. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA (The Journal of the American Medical Association). 281(8):736-8.
- Albert X, Huertas I, Pereiro, Sanfelix J, II, Gosalbes V, Perrota C. Antibiotics for preventing recurrent urinary tract infection in non-pregnant women. Cochrane Database Syst Rev.
- Claire Duvallet, Sean M. Gibbons, Thomas Gurry, Rafael A. Irizarry & Eric J. Alm. Meta-analysis of gut microbiome studies identifies disease-specific and shared responses, Nature Communications 8, Article number: 1784 (2017)
- Stapleton A. Novel approaches to prevention of urinary tract infections. Infect Dis Clin North Am. 2003;17(2):457–71.
- Amdekar S, Singh V, Singh DD. 2011. Probiotic therapy: immunomodulating approach
toward urinary tract infection. Curr Microbiol. 63(5):484-90 - Sarah Cribby, Michelle Taylor, and Gregor Reid, Vaginal Microbiota and the Use of Probiotics, Interdisciplinary Perspectives on Infectious Diseases
Volume 2008 (2008), Article ID 256490 - Anukam K, Osazuwa E, Ahonkhai I, Ngwu M, Osemene G, Bruce AW, Reid G. 2006.
Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral
probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized,
double-blind, placebo-controlled trial. Microbes Infect. 8(6):1450-4. - Kontiokari T, Laitinen J, Järvi L, Pokka T, Sundqvist K, Uhari M. 2003. Dietary factors protecting women from urinary tract infection. Am J Clin Nutr. 77(3):600-4.
- Beerepoot MA, ter Riet G, Nys S, van der Wal WM, de Borgie CA, de Reijke TM, Prins JM, Koeijers J, Verbon A, Stobberingh E, Geerlings SE. Lactobacilli vs antibiotics to prevent urinary tract infections: a randomized, double-blind, noninferiority trial in postmenopausal women. Arch Intern Med. 2012 May 14;172(9):704-12.
- Bodel PT, Cotran R, Kass EH. 1959. Cranberry juice and the antibacterial action of hippuric acid. J Lab Clin Med. 54:881-8
- Ofek I, Goldhar J, Zafriri D, Lis H, Adar R, Sharon N. 1991. Anti-Escherichia coli adhesin activity of cranberry and blueberry juices. N Engl J Med. 324(22):1599.
- D-Mannose for Bladder and Kidney Infections by Jonathan Wright, MD, Editor, Nutrition and Healing, Tahoma Clinic Blog, D-Mannose for Bladder and Kidney Infections
- Walker EB, Barney DP, Mickelsen JN, Walton RJ, Mickelsen RA., Jr Cranberry concentrate: UTI prophylaxis. J Fam Pract. 1997;45(2):167–8.
- Stothers L. A randomized trial to evaluate effectiveness and cost effectiveness of naturopathic cranberry products as prophylaxis against urinary tract infection in women. Can J Urol. 2002;9(3):1558–62.
- Kranjčec B1, Papeš D, Altarac S, D-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial, World J Urol. 2014 Feb;32(1):79-84.